-
Category
Craniomaxillofacial Surgery
Orthopedic Surgery
Spine Surgery
Orthopedic Implants
Hip Surgery
Knee Surgery
Pectus Excavatum
Bone Graft
Disinfectants
Healthcare
What is endoscopic discectomy?

Endoscopic discectomyis one of the effective surgeries for removing herniated disc materials. In endoscopic discectomy procedure a herniated disc is removed by microscopic instruments inserted through the endoscope.
One of the effective surgeries for removing herniated disc materials is called endoscopic discectomy. In this procedure a herniated disc is removed by microscopic instruments inserted through the endoscope.
A brief history: In 1990, Parvis Kambin described anatomical safe zone that made the field of endoscopic spine develop to the technique of percutaneous nucleotomy (a needlelike material is used in this project). This matter gradually led to creating larger materials but nowadays in endoscopic discectomy a laser is applied for cutting the nerves grown in the tear of the layer of the disc and it also helps to compress the tears without damaging the disc.
Let's know what is endoscopic discectomy and how it can helps to traatment.
What are the advantages and disadvantages of endoscopic discectomy?
Advantages: One of the considerable authority about endoscopic disc surgery is its high success rate (up to 90%). Spinal fusion is not needed in this procedure. HD cameras are used to provide a clear view of injured areas for operator. The smallest size possible in endoscopic discectomy technique reduces the risk of scarring (almost ¼ inch)
And it also has low risk for great volume of bleeding so the patient can spend less recovery time with less pain (Dependence on narcotic and opioid substances lowers to its minimum) Spinal portability is conserved because it contains less scarring and tearing of muscle tissues, also general anesthesia is not needed because conscious sedation is sufficient. And ultimately the patient can get back to his former activity.
Disadvantages of percutaneous endoscopic lumbar discectomy are a lack of sufficient radicality due to ossification of the hernia and complicated anatomy of the intervertebral foramen in clinical cases. Excellent clinical outcome of large case series after PELD (Percutaneous Endoscopic Lumbar Discectomy) surgery is reported. However, we need to face the limitations and complications of the surgery. The complication rate should be reduced by caring about the treatment, surgical indications strictly selected and the guidance of experienced surgeons.
What conditions can an endoscopic discectomy surgery treat?
About 90% of acute sciatica attacks better with controlled management; thus, the main therapy for a patient with symptomatic lumbar disc herniation continues to be nonoperative type of treatments, such as prescribing anti-inflammatory medications, physical therapy, and lumbar injection, but if the patient has an acute or accelerating neurological deficit other procedures should be considered. Some conditions like altered bladder and bowel function and ongoing neurological deficiency (for example: sensory deficit in the lower extremities and motor weakness) indicates endoscopic lumbar discectomy, also for some patients with radicular pain that lasts after an adequate plan of conservative management we should consult surgery treatments.
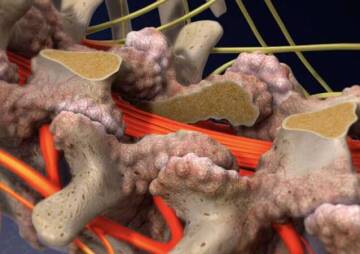
PELD is an efficient and safe treatment for lumbar disc herniation, lumbar spinal stenosis, frequent lumbar disc herniation, and other lumbar diseases; for example severe discogenic low back pain caused by degenerative disc disease, segmental instability, postlaminectomy instability, multiple recurrent disc herniations, foraminal stenosis associated with deformity and degenerative scoliosis, spinal injury or pseudarthrosis. There are some other complications that PELD can be advantageous for, Such as dural tear, nerve root injury, recurrence, and so on.
Endoscopic spine surgery for soft disc herniation can be helpful with benefits of minimal tissue trauma in properly selected cases. Given the recent technical advancements, the surgical indications for endoscopic spine surgery are still developing and the clinical results have become more practical and valid.
How is an endoscopic discectomy surgery performed?
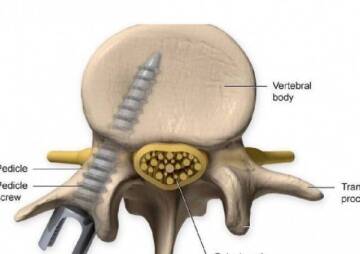
Endoscopic discectomy is an outpatient surgical procedure. Commonly the surgeon exerts a local anesthetic so the patient doesn't feel any pain during the surgery. After the patient gets numb, an incision will be made around the herniated disc and through muscle tissue in his back and with the help of X-ray fluoroscopy and magnified video for guidance, a tiny, specifically designed endoscopic probe is inserted between the vertebrae and into the herniated disc space. (An HD camera/endoscope is used in order to provide a vivid view of herniated disc for surgeon and make an assessment of what needs to be removed). Meanwhile, a dilator is interpolated to keep the incision open with a 1/4 inch metal tube giving the surgeon access to the disc. Microscopic surgical attachments are sent down the void center of the probe to remove the offensive fragment of the disc. The microsurgical supplements can also sometimes be used to push the bulging disc back into its former place and be used for the removal of disc fragments and narrow bony spurs. Once the procedure is complete with any tears plugged and herniated discs removed, the metal tube is taken out and the surgeon will close the incision.

What are types of endoscopy procedure?
One of the Endoscopic discectomy techniques for lumbar surgery is:
intra-foraminal procedure
First of all, we need a well cushioned and supportive radiolucent frame or gel role to lay out the patient in the prone position. Almost in all cases, local anesthesia with intravenous sedation can be applied. But if general anesthetic is to be used necessarily, spinal cord monitoring as well as tactile posterior thigh palpation should be considered to evaluate the nerve center impingement by operative interference.
Two intra-foraminal approaches (intra-discal and extra-discal) are generally used. At the first step of an intra-foraminal extra-discal approach, three skin markings should be defined using fluoro-scopic imaging. Thus, in the true AP(antero-posterior) fluoroscopic view a linear midline sign should be drawn on the patient's skin. And then, on a true orthogonal oblique view, the disc space is determined. As the third mark, a clear line should be defined in the posterior facet part that is also drawn in the lateral fluoroscopic view. The entrance part of the skin for the spinal needle should be no more posterior than the posterior facet line at the junction of the lateral line and the posterior facet line. The more intra-foraminal position of the area that is needed, the closer to the posterior facet line the entrance part should be for the spinal needle import. An 18 degree spinal needle is then located on the posterior edge (oblique view) of the disc space and no further medial than the medial pedicle line (antero-posterior angle)
Now that we explored an intra-foraminal intra-discal approach as described by is planned, the same three skin signs are marked as in an extra-discal type of endoscopic discectomy and an extra fourth skin sign is made (this mark is suggested by Yeung in his previous surgical technique) .In order to draw this mark the surgeon positions the apex of the metal marker in the axis of the disc space on the lateral orthogonal view and then he draws a mark on the metal marker close to where the posterior skin extends anterior. Then the space between the midline skin and the entrance part of the needle should be marked. The spinal needle is then placed in the posterior ¼ of the disc space (lateral view) and in the central disc (AP view). After fixing the needle location, a mixture 2ml of indigo carmine and 8 ml of omnipaque is injected as necessary for doing the process of discography and to blemish degenerative nucleus material. In case that multi-focal disc herniation is diagnosed, a needle entrance area is placed usually between the intra and extra discal skin entry points and has a distal to proximal aptitude. The intra discal endoscopic discectomy should be performed first followed by extra-foraminal decompression
After spinal needle location is arranged, in either the intra or extra discal technique, a 1 mm guide wire is practiced through the spinal needle. An obturator with two foramen is placed over the guide wire followed by working cannula placement (7 mm or 8 mm). Ultimately, the endoscope should be placed into the working cannula (a thin elastic tube). Correct discectomy and post- decompression affirmation of epidural pulsation is performed. Evidence of epidural pulsation approves spinal content decompression. Most of the time, direct vision of the cross nerve root is not always required to confirm decompression. Surgeons permit visualization of the existing nerve root by dissolving the working cannula and endoscope into an extra discal. The appropriate utilization of bipolar coagulation, focused lasers and endoscopic discectomy burrs allow for discectomy as well foraminoplasty and intervertebral fusion employing expandable cage technology.
Inter-laminar procedure
The posterior inter-laminar approach in endoscopic disc surgery is utilized predominantly at the L5-S1 level in order to make paracentral discectomies practicable. An antero-posterior view of the L5-S1 level should be provided for marking the intended points. A second line must be drawn just lateral to the midline. At this junction a tiny incision (4 mm can be sufficient) is made and an obturator with two foramen is applied down to the level of the ligamentum flavum (LF). The next move is placing the working cannula and endoscope. As you might have noticed, a guide wire is not helpful. Accurate dissection through the ligamentum flavum is then performed. Also a partial facetectomy may occur for identifying the lateral edge of the S1 nerve root (in some cases this act might be needed). The working cannula is then rotated and the S1 nerve is gently retracted. Finally endoscopic discectomy surgery can then be performed.

What postoperative care is necessary?
Activity in General:
- You can only lie on a hard mattress, and never lean on couches or recliner chairs.
- You can lie on your back or side, but never on your abdomen.
- If sitting, use only a straight back comfortable chair to ensure the right support not to exceed a half hour at a time. You can raise your sitting time gradually.
- Obviously no stooping, bending, pushing, lifting or straining.
- Avoid housework, exclusively vacuuming the house and sweeping.
- Therefrom you might be tired post-operatively, Health care providers suggest 2-3 naps daily.
- You can continue cooking as long as you are not lifting anything heavier than 10 pounds.
- Consider proper body mechanics to maintain your neutral spine position.
- Increasing pain is a red alert warning you to rest.
- DO NOT involve yourself in tough activity for at least 10 weeks after surgery.
1st Week Post-Operative:
- You may need to climb stairs with helping hands or assistance.
- You may ride in a vehicle as a passenger, but never driving and no long road trips. Also it's important to keep the time in the car less than 20 minutes.
- Take pain killer supplements as directed, don’t try to “tough it out.” You will heal sooner if you feel better.
- Take a walk around your home on a smooth, flat surface. Try to be ambulating half of the day.
- Do not lift anything heavier than 10 pounds.
2nd Week Post-Operative:
- Light housework but still no vacuuming or sweeping.
- You can drive less than 20 minutes at a time if it doesn't make you feel uncomfortable as a passenger.
- Make sure to make your first post-operative visit.
- May your health care provider recommend an exercise program at your first visit after endoscopic discectomy.
- Increase your walking to 1 mile per day if tolerated well.
- Avoid sexual activity at this period of time.
-3rd Week Post-Operative:
3rd Week Post-Operative:
- It's ok to use a hot tub or spa if you are “scab free.”
- Increase walking time and housework as long as you are not teased.
- In this section you can get back to your sexual activity if relatively pain free.
- If you need to lift anything, still better to be careful and not to exceed 25 pounds and use proper body mechanics.
4th Week Post-Operative:
- Raise driving time as tolerated.
- Return to work will be discussed with your doctor because this matter is different from patient to patient.
- Slowly increase walking to 1-2 miles daily or as tolerated.
- Increase housework as tolerated.
What is the success rate of endoscopic discectomy?
Reliable follow-up research and our in-house observations show that endoscopic discectomy surgery is a highly successful operation. A study that observed the post-surgical condition of patients over a 10-year period showed that more than 80% reported magnificent results and none had any poor results.