-
Category
Craniomaxillofacial Surgery
Orthopedic Surgery
Spine Surgery
Orthopedic Implants
Hip Surgery
Knee Surgery
Pectus Excavatum
Bone Graft
Disinfectants
Healthcare
Craniotomy for Tumor Resection: Reasons, Risks, and Types
Scarier than brain tumor is the thought of surgeries and all the stories and myths from people who underwent brain surgery, craniotomy for tumor resection, or any other type of surgical treatment. But what is craniotomy for tumor resection? Is it as scary as some people think? Follow us to find the answers.
Having a brain tumor can be a scary thing. Scarier than that is the thought of surgeries and all the stories and myths from people who underwent brain surgery, craniotomy for tumor resection, or any other type of surgical treatment. But what is craniotomy for tumor resection? Is it as scary as some people think?
What Is a Craniotomy?
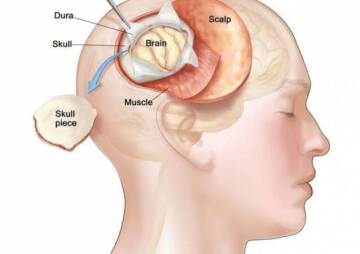
Sometimes accessing a brain tumor is more complicated than removing it. Hence, some extra steps must be added to help the surgeon access cancer in the brain. One of these methods is a craniotomy surgery, which includes a bone-removal step in addition to levels of other brain surgeries.
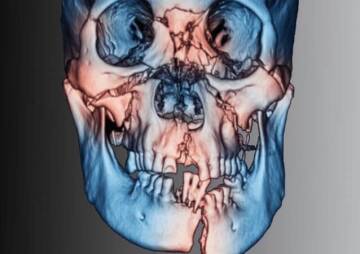
In a craniotomy, the brain surgeon removes part of the skull bone to access a tumor. Craniotomy resection may require computer and imaging assistance to find and reach the exact location of cancer. Naturally, magnetic resonance imaging [MRI] or computerized tomography [CT] scans are the techniques that come in first.
The removed part of the skull bone is called a "bone flap," which is put back in place after the craniotomy excision of the tumor. Typically, the bone flap is replaced at the end of the procedure with tiny plates and screws. There are cases where the bone flap is not returned, but that is a different brain surgery called "craniectomy," which will be discussed further in eth article.
The name of the craniotomy surgery is derived from the skull (cranium) to be removed. The size and complexity of a craniotomy depend on the patient's problem, which can range from brain swelling to taking out foreign objects, like bullets.
Reasons for a Craniotomy
Why does a person need to undergo craniotomy and resection? As briefly mentioned above, reasons for a craniotomy surgery vary and include, but are not limited to:
- Accessing the treatment site for diagnosing or removing tumors
- Relieving intracranial pressure by eliminating damaged or swollen areas of the brain may have been caused by traumatic injury or strokes
- Device implantation for purposes like treating movement disorders, such as Parkinson's disease or dystonia (a type of movement disorder), or refractive epilepsy
- Clipping or repairing of an aneurysm
- Removing blood or blood clots from a leaking blood vessel
- Draining a brain abscess (an abscess is an infected pus-filled pocket in the tissue)
- Repairing skull fractures
- Repairing a tear in the membrane lining the brain (dura mater)
- Taking out a foreign object, for example, a bullet
Craniotomy and resection are not used only for tumors, as explained above. Whenever the brain is under too much pressure, like when it is swollen, has blood clots, or has an abscess, craniotomy surgery is the choice. If craniotomy excision of the tumor, blood clots, a bullet in the head, or for any other reason is the treatment, how should the patient prepare?
Preparing for a Craniotomy
Before a craniotomy surgery, the patient must stop taking any kind of non-steroidal anti-inflammatory medicines and blood thinners, at least one week earlier. However, if there are medicines explicitly prescribed for the surgery, they should be carefully taken according to the schedule. Further, the patient should not eat or drink from the night before the surgery.
Smoking and drinking alcohol are also prohibited from one week before to two weeks after the surgery. If MRI or CT-Scans are required, fiducials might be placed on the patient's forehead and behind the ears to help align the preoperative MRI to the image guidance system. In many cases, the doctor needs blood tests to assure the patient's health.

A craniotomy resection is done under general anesthesia, regardless of the type of the surgery. Signing a consent form is a must, and the patient should read the way carefully and know what they are undergoing. They should also know the risks associated with such brain surgeries.
Risks of A Craniotomy
After a craniotomy excision of a tumor or a craniotomy for other reasons, a patient might experience swelling and bruising in the face or around the eyes, headache, dizziness, and problems with memory, speech, or vision. Thus, the neurosurgeon specifies how many days the patient needs to spend in an intensive care unit (ICU), where the heart rate, blood pressure, and neuro signs are constantly monitored. Despite all these precautions, the patient might still undergo post-surgery risks.
The general post-surgery risks are also present here: bleeding, infection, blood clots, and reactions to anesthesia. In the case of craniotomy surgery, some other dangers are also added, depending on the type of the procedure:
- Strokes
- Seizures
- Swelling of the brain
- Nerve damage
- CSF leak or leakage of cerebrospinal fluid, which is the fluid that surrounds and protects the brain
- Loss of some mental functions
- Pneumonia, which is a kind of lungs' infection
- Unstable blood pressure
- Muscle weakness
Besides, some risks are method-specific and do not happen to all patients after a craniotomy. They depend on the severity and complexity of the problem and include:
- Memory problems
- Speech difficulty
- Paralysis
- Abnormal balance or coordination
- Coma
Post-surgery care can prevent or reduce some of the risks, but usually, the patient needs to compromise and undergo surgery knowing these could happen. In many cases, it is a matter of life or death, and the patient has no other choice.
Different Types of Craniotomy
Like any other type of brain surgery, craniotomy also has different kinds, ranging from right frontal craniotomy for tumor resection to translabyrinthine craniotomy. The model is chosen based on the patient's conditions, the purpose of the surgery, and the overall benefits. Some of the main types of craniotomy are as follows:
Extended Bifrontal CraniotomyWhen minimally invasive approaches fail to meet the needs of surgery, the surgeon can choose extended bifrontal craniotomy. Here, an incision is made in the scalp behind the hairline and the bone that forms the contour of the orbits, and the forehead is removed.
The most common purpose is to reach difficult tumors toward the front of the brain. It is a traditional skull base approach with the core belief that removing extra bone is safer than unnecessarily manipulating the mind. Usually, meningiomas, esthesioneuroblastomas, and malignant skull base tumors are treated by extended bifrontal craniotomy. In the end, the bone flap is replaced.
-
Minimally Invasive Supra-Orbital "Eyebrow" Craniotomy
Supra-orbital craniotomy, usually known as "eyebrow" craniotomy, is another procedure to remove brain tumors. As the name suggests, it is a minimally invasive approach and includes a small incision within the eyebrow to access tumors in the front of the brain. Rathke's cleft cysts, skull base tumors, and several pituitary tumors can also be treated by this method.
As it is a minimally invasive procedure, it can be less painful than open craniotomy surgeries. The recovery period might be shorter, and no big scar is left in the surgery place.
-
Retro-Sigmoid "Keyhole" Craniotomy
Retro-sigmoid craniotomy, often known as "keyhole" craniotomy, is another minimally invasive surgical procedure to remove brain tumors. After a small incision behind the ear provides access to the cerebellum and brainstem, the surgeon can remove the skull base tumor. Meningiomas, acoustic neuromas, and metastatic brain or spine tumors are the other targets of keyhole craniotomy.
Like other minimally invasive approaches, retro-sigmoid craniotomy also needs less recovery time, while it leaves a minimal surgery scar and less pain compared to different types of brain surgery.
-
Orbitozygomatic Craniotomy
The orbitozygomatic craniotomy is the second traditional skull base approach introduced in our article. Like extended bifrontal craniotomy, orbitozygomatic craniotomy is also used to access and operate difficult tumors and aneurysms. This approach's founding belief is also the same as that of extended bifrontal craniotomy: removing extra bone is safer than unnecessarily manipulating the brain.

When minimally invasive approaches cannot help, the bone that forms the contour of the orbit and cheek is removed to be replaced at the end with the purpose of craniotomy excision of the tumor. Some cases that can be treated using this type of surgery include craniopharyngiomas, pituitary tumors, and meningiomas. The neurosurgeon can reach deeper and access difficult parts of the brain while minimizing severe damage to the brain.
-
Translabyrinthine Craniotomy
In the translabyrinthine craniotomy, an incision is made in the scalp behind the ear to remove the mastoid bone and some of the inner ear bone. An essential part of the inner ear bone that is removed here is the semicircular canals containing receptors for balance. Sometimes the whole tumor cannot be removed due to the severe damages that the removal procedure can create. However, the neurosurgeons usually try to remove the entire tumor or as much of it as possible.
The biggest problem with this method is the loss of hearing. When the semicircular canals are removed, hearing is sacrificed to access and remove the tumor. Nevertheless, the risk of facial nerve injury can be reduced.
In all of these methods, the removed bone flap is replaced and held in place with screws and plates. This is not always the case with bone flap, and sometimes the surgeon does not replace the bone.
Craniotomy, Craniectomy, and Cranioplasty
A craniotomy, a craniectomy, and a cranioplasty sound similar but are three different techniques of brain surgery. As the names suggest, the cranium (skull) is involved in all the three methods. As mentioned before, in a craniotomy, a part of the head is removed temporarily to allow access to deeper parts of the brain for removing tumors, blood clots, brain swelling, foreign objects, and treating some other problems, as mentioned in the previous sections of the article. The bone flap is put back in place at the end of the surgery and is fixed by titanium plates and screws.

On the other hand, in a craniectomy, the bone flap is not replaced immediately. Usually, neurosurgeons prefer this method when the problem is traumatic brain injuries and other head injuries that include swelling. The removed part of the skull is kept away to lessen the pressure and compression of some regions of the brain.
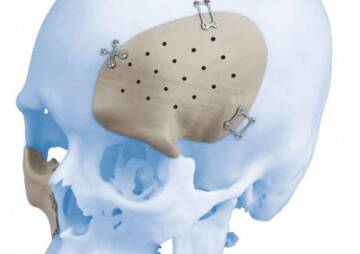
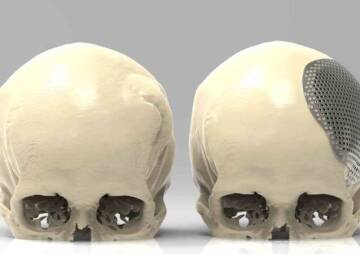
In the third technique, cranioplasty, the bone flap is removed like the previous two methods. However, it is never reattached since the removed part of the skull has problems on its own: it is damaged or cancerous. Thus, the removed portion is replaced with titanium, acrylic, or a synthetic bone substitute. Installing the new piece should also be done by a neurosurgeon.
Pressure relief in an emergency is among the top benefits and specific characteristics of cranioplasty. It can save lives with this particular benefit. Another cranioplasty-specific benefit is that the new bone piece can help restore the skull's natural contour. Sometimes the removed part misshapes the skull, but cranioplasty can help regain the natural shape. Titanium implants are specifically preferred for cranioplasty due to their numerous advantages.
Use of Titanium Implants in Cranioplasty
As mentioned in the previous section, in a cranioplasty, the removed part of the skull cannot be put back. It is either damaged or cancerous or has other problems and should not be replaced. Thus, an implant made of titanium, PEEK, acrylic, or a synthetic bone substitute must be used.
Titanium is one of the most common materials used for operational purposes and implants. It is also becoming more popular in cranioplasty, because it prevents cosmetic deformity, reduces the vulnerability of unprotected brain tissues, and minimizes the risks and costs associated with additional surgeries and procedures.

The brain surgery can be a minimally invasive approach like the eyebrow craniotomy, a right frontal craniotomy for tumor resection, or a cranioplasty, where a part of the skull is thrown away, and a piece of titanium or other materials replaces it. Nonetheless, the patient must know enough about the surgery, preparing for it, and its risks to reduce the post-surgery dangers as much as possible.