-
kitengo
Craniomaxillofacial Surgery
Orthopedic Surgery
Spine Surgery
Orthopedic Implants
Hip Surgery
Knee Surgery
Pectus Excavatum
Bone Graft
Disinfectants
Healthcare
Osteoporosis and fractures of the spine, a silent but dangerous disease
Osteoporosis causes the bones to become weak and fragile. These fractures most often occur in the thigh, wrist or spine. In this article, we will focus specifically on osteoporosis in the spine.
Osteoporosis causes the bones to become weak and fragile, so fragile that the bones crack even with a simple fall or small pressures such as bending, hugging, or coughing and sneezing. These fractures most often occur in the thigh, wrist or spine. But in this article, we will focus specifically on osteoporosis in the spine.

How does osteoporosis develop?
Bone is a living tissue that is regularly regenerating. Osteoporosis occurs when new bone tissue is not aligned with old bone tissue. This complication is common in men, women and children of all colors and races, but in general white and Asian women and postmenopausal women are more likely to have this problem. Medications, a healthy diet, and certain exercises can help prevent bone loss or strengthen weak bones.
You can learn more about osteoporosis to have less painful aging .
Osteoporosis and fractures of the spine
When osteoporosis weakens bones, the bones are more likely to crack or break, even the bones of the spine. The spine is one of the most common sites of bone fractures due to osteoporosis. These spinal fractures are also called compression vertebral fractures. Imagine that each bone in your spine is a square block. When a bone breaks, it is as if one of these boxes has been squeezed or flattened. This can happen in one or more vertebrae of the back. This results in severe back pain when standing, walking, sitting or lifting objects.

As you grow older, your bones become thinner and weaker, and your chances of developing osteoporosis increase. As a result, women, especially those over the age of 50, are more likely to have a broken spine. According to statistics, at the age of 80, about 40% of women develop osteoporosis, and when osteoporosis is more, the risk of spinal fractures is higher.
To prevent these fractures, the best way to prevent osteoporosis is to increase the strength of the bones and, of course, treat cracks and vertebral fractures.
Symptoms of a spinal fracture
Many people complain of back pain when they have a broken spine, but many have no symptoms. About two-thirds of fractures of the spine are painless, which makes it a little harder for doctors to diagnose. But over time, different symptoms appear in the patient.
In general, fractures in the lower spine cause more pain and movement problems than in the upper spine. Why? Compression fractures of the vertebrae usually occur near the waistline as well as slightly above it (mid-chest) or below it (waist), and pain is more common in these areas.
This pain often gets worse with movement, especially when changing position. It is often relieved by resting or lying down. Coughing and sneezing can also increase pain. Although the pain may spread to other parts of the body (such as the abdomen or lower legs), it is not uncommon.

The most common symptoms of a spinal fracture are:
- Sudden and severe back pain
- Pain that gets worse when standing or walking
- Problems with bending or twisting the body
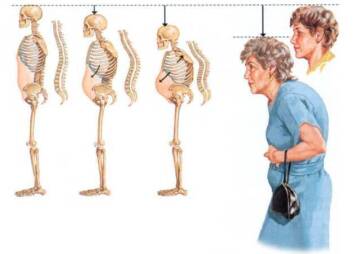
- Shortening height
- Hunched back
How is a spinal fracture diagnosed?
To diagnose the cause of the pain, the doctor begins treatment with a clinical examination. Examines the alignment or smoothness of the spine and its condition. Presses on specific areas of the back to determine if the pain is from a muscle or bone injury. To make sure the spinal nerve is not damaged, your doctor will do a neurological examination and check for numbness, changes in reflexes, or muscle weakness.

The next step is imaging tests, which provide important information about the fracture to the doctor and allow the doctor to determine if the injury is new (acute) or older (chronic).

To diagnose a spinal fracture, they scan the bone using X-rays or computed tomography (CT) scans. Bone density test A dual X-ray absorption scan (DXA or DEXA) is also performed to get enough information about the condition of the bones.
MRI shows in more detail any damage to the soft tissues around the fracture (nerves and disc). Because of how the bone is shown, MRI helps the doctor determine the age of the fracture. In the case of a new fracture, the affected bone appears brighter than the surrounding bone. This indicates inflammation in the area. If the fracture is old, the bone looks normal.
Treatments for spinal fractures due to osteoporosis
Non-surgical treatments
Fortunately, most people with compression fractures heal within three months without the need for special treatment to repair the fracture. Simple measures, such as a short rest period and limited use of painkillers, are all that the patient needs to do. Patients are usually encouraged to do light exercise such as swimming or walking as soon as they can move. In some cases, the use of braces is recommended to limit sudden and unusual movement and improve vertebral fractures.

But if the fracture is associated with osteoporosis, the patient is at greater risk. In this case, in addition to the usual treatments for fractures, doctors must also treat osteoporosis.
Patients with osteoporosis should be evaluated with a bone mineral density test, and osteoporosis should be treated with standard osteoporosis medications such as alendronate bisphosphonate (Fosamax), Actonel and Boniva. Bisphosphonates can help reduce acute pain, but their main benefit is improved bone mineral density. In the long run, they can reduce the rate of new vertebral fractures by up to 50%.

Another bone drug, calcitonin (myacalcin, fortical), is less effective in improving bone mineral density but can relieve some pain, although it is not a substitute for painkillers. It is an injectable bone repair medicine (forteo), increases bone mineral density and reduces the risk of vertebral fractures.
Surgical treatment
If the pain and fracture are severe and non-surgical treatment is unresponsive, your doctor may recommend surgery.
In the past, the only options for vertebral fracture surgery were the vertebral compression fractures. Which required extensive surgery but today uses less invasive methods.
There are two methods of strengthening the vertebrae of the spine called kyphoplasty (kyphoplasty) and vertebroplasty (vertebroplasty). Patients suffering from pain from vertebral fractures are usually candidates for treatment with these methods. However, a person with a pressure fracture of more than 70% of the height of the vertebral region is not a good candidate for these two methods.

In kyphoplasty, a needle is inserted into a broken vertebra using X-rays. Then a small device called a balloon is inserted through the needle into the broken nut. The balloon is inflated from inside the nut, which causes the height and shape of the nut to return to its original size, then this part of the balloon is removed and the empty space is filled and reinforced with special cement materials. This operation can be performed under general anesthesia or local anesthesia, and the patient can return to daily activities one day after the operation.

Vertebroplasty is a technique similar to kyphoplasty, but does not use balloons to create empty space. Instead, cement is injected directly into the nut fracture. After this surgery, patients are encouraged to return to their normal routine as soon as possible.
Treatment of compression fractures of the vertebrae by spinal fusion method
Sometimes, compression fractures of the vertebrae do not heal properly. In such a case, the spine surgeon may suggest a method known as spinal fusion. In this surgical procedure, two or more vertebrae are connected. This surgical procedure is performed with precision instruments such as pins, implants, rods and other equipment, usually made of titanium or stainless steel .

Can people with osteoporosis have spine surgery?
Managing patients with osteoporosis who require spinal surgery is challenging because of its potential side effects. Treatment for these people should be accompanied by several other treatments that require specialists including a spine surgeon, primary care physician, endocrinologist, and physiotherapist.
These patients should receive calcium and vitamin D. Hormone replacement therapies, including estrogen receptor modulators, should be considered for elderly female patients with osteoporosis. Bisphosphonates, or intermittent parathyroid hormone, are prescribed for people with significant osteoporosis of the spine and affect bone regeneration before treatment with anti-absorption drugs.

Usually, people with multiple vertebral fractures do not have the problem of vertebroplasty or kyphoplasty and need to use vertebral fusion surgery. But many spinal implants require strong bones to hold the spine in place. Patients with osteoporosis may have difficulty with this. Complications of spinal fusion are more common in patients with osteoporosis over 65 years of age. Also, less bone repair (fusion) has been observed in patients with osteoporosis. It is significantly more difficult to fix the spine in weak bone
The most common early complications of postoperative osteoporosis are pulling or loosening of the pedicular coils, pedicle fractures, and pressure fractures of the lateral vertebrae. Sometimes, even after three months, you will see the bars move out of place. In this situation, they often use larger and stronger screws to stay in place. Even extra bone grafts may be needed to ensure fusion, and other products are helpful in helping fusion (such as BMP). At the same time, the patient needs to use a lumbar brace for a longer period of time after surgery.
And finally, what happens if osteoporosis is not treated?
The cumulative effect of multiple fractures can be devastating. Chronic pain, inability, and difficulty performing the normal activities of daily living can lead to isolation, relationship problems, and emotional problems, including depression. Spinal fractures due to osteoporosis also increase the risk of premature death.
Most people who suffer from vertebral fractures due to osteoporosis have these fractures in the chest area (mid-back) and lower back (back). One or two fractures may cause a slight reduction in height, but multiple fractures can lead to a curvature or so-called hump, which in addition to appearance also affects a person's mobility and health. Sometimes these fractures become so painful that they prevent a person from moving properly. The patient will need a walker and a cane to walk and will not be able to sit for long periods of time.

As a result of these fractures, the spine gradually becomes more disordered. The upper body comes forward and rounds. The space between the ribs and the pelvis closes. The chest wall is narrow and the abdominal organs are crushed, causing the abdomen to bulge forward. In very severe cases, breathing may be difficult and digestion may be impaired. All of these conditions reduce the quality of life and in acute cases will lead to death.
- vitambulisho osteoporosis