-
kitengo
Craniomaxillofacial Surgery
Orthopedic Surgery
Spine Surgery
Orthopedic Implants
Hip Surgery
Knee Surgery
Pectus Excavatum
Bone Graft
Disinfectants
Healthcare
Spinal Fusion Surgery Success Rate

Spinal fusion surgery success rate varies between 70% and 95%, and there are several factors that will impact the success rate of the surgery.
This article views spinal fusion surgery success rate from two aspects. First aspect is related to the type of degenerative disc disease, second aspect is other factors related to success of surgery such as failure of solid fusion after spine surgery, implant failure in spine surgery, transfer lesion to another level after a spine fusion.
The Type of Degenerative Disc Disease and Spinal Fusion Surgery Success Rate
Spinal fusion surgery success rate varies between 70% and 95%, and there are several factors that will impact the success rate of the surgery, including:
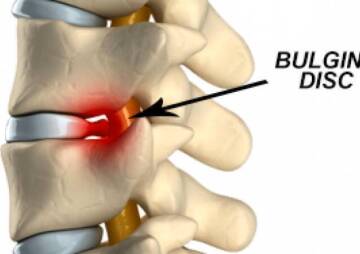
Spine fusion for conditions that arise from gross instability (e.g. isthmic or degenerative spondylolisthesis) tends to be more successful than surgery done for pain alone (e.g. degenerative disc disease).
Individuals with only one badly degenerated disc (especially L5-S1) but an otherwise a normal spine tend to fare better than those undergoing multilevel fusions. Fusion surgery is generally considered for one or possibly two levels, and multilevel fusions should be avoided except in cases of severe deformity.
Individuals who have significant disc degeneration usually find more pain relief from a fusion than those with only minor degeneration on the MRI scan (e.g. still have a tall disc).
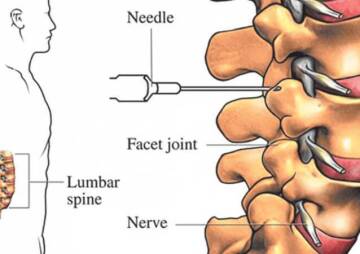
The most important success factor is confirming that a patient’s back pain is truly caused by degenerative disc disease, rather than some other condition. This is done by a combination of a careful review of the patient’s history, a physical exam, and diagnostic tests (such as x-ray and MRI), and/or possibly a discogram.
There are also other reasons for a spinal fusion surgery to be successful or not, including fusion and implant failures, and transfer lesions.
Failure of Solid Fusion After Spine Surgery
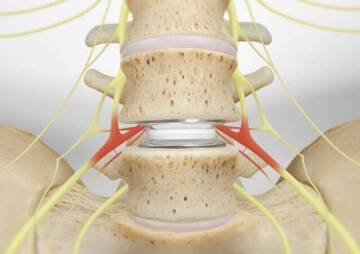
When the fusion is for back pain and/or spinal instability, there is a correlation (although weak) between obtaining a solid fusion and having a better result of the spine surgery. If a solid fusion is not obtained through the spine surgery, but the hardware(orthopedic implant) is intact and there is still good stability to the spine, the patient may still achieve effective back pain relief with the spine surgery. In many cases, achieving spinal stability alone is more important than obtaining a solid fusion from the spine surgery.
Implant Failure in Spine Surgery
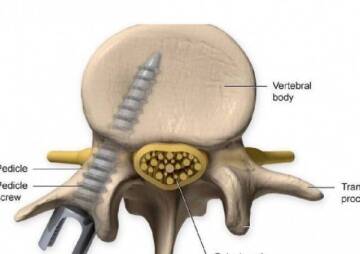
An instrumented fusion can fail if there is not enough support to hold the spine while it is fusing. Therefore, spinal hardware (e.g. pedicle screws, available in Health News Center) may be used as an internal splint to hold the spine while it fuses after spine surgery. However, like any other metal it can fatigue and break (sort of like when one bends a paper clip repeatedly). In very unstable spines, it is therefore a race between the spine fusing (and the patient’s bone then providing support for the spine), and the metal failing.
Metal failure (also called hardware failure, implant failure), especially early in the postoperative course after back surgery, is an indicator of continued gross spinal instability. The larger a patient is and the more segments that are fused, the higher the likelihood of implant failure. Implant failure following spine surgery should be very uncommon in normal sized individuals with a one level fusion.
Transfer Lesion to Another Level after a Spine Fusion
A patient may experience recurrent pain many years after a spine fusion surgery. This can happen because the level above or below a segment that has been successfully fused can break down and become a pain generator.
This degeneration is most likely to happen after a two-level fusion (e.g. a fusion for L4-L5 and L5-S1 levels) and in a young patient (in the 30-50-year-old age range).
It is much less likely to happen if only the L5-S1 level is fused, as this segment typically does not have much motion and fusing this level does not change the mechanics in the spine all that much.
Most of the motion in the spine is at the L4-L5 level, and to a lesser extent at L3-L4. When the L4-L5 level is included in the spine fusion it transfers a lot of stress to L3-L4. This does not present as much of a problem for elderly patients, since they tend to not be as active nor do they have the fusion for as many years.
Transfer lesions are far more common in degenerative osteoarthritis conditions ( e.g. degenerative spondylolisthesis) and far less common in disc degeneration problems.
Other health factors or activities can undercut the chances of obtaining a successful fusion, and should be treated or controlled prior to surgery if possible. These include smoking, obesity, malnutrition, osteoporosis, chronic steroid use, diabetes mellitus or other chronic illnesses.
A surgeon will consider different techniques and both anterior (from the front) and posterior (from the back) approaches to perform the fusion.